Abstract

Invasive fungal disease (IFD) is a significant cause of morbidity and mortality in patients undergoing allogeneic haematopoietic stem cell transplantation (allo-HSCT). Recent data from large CIBMTR and EBMT studies have reported the impact of pre-existing IFD (pre-IFD) on allo-HSCT outcomes. The aim of this study was to analyse the impact of pre-IFD on overall survival (OS) and IFD free survival in patients with myeloid malignancies and aplastic anaemia who underwent allo-HSCT.
Methods: A large single centre retrospective analysis was performed on patients with myeloid malignancies and Aplastic anaemia (n=369) who consecutively underwent allo-HSCT between Jan 2012 and June 2016. IFD was defined by published EORTC criteria as possible, probable and proven disease. Patients with pre-IFD (n=76) i.e. with history of actively treated IFD within 3 months of HSCT, were compared with those without pre-IFD (n=293). Majority of patients (97%) were taking newer tri-azole prophylaxis (posaconazole) as per standard centre protocol.
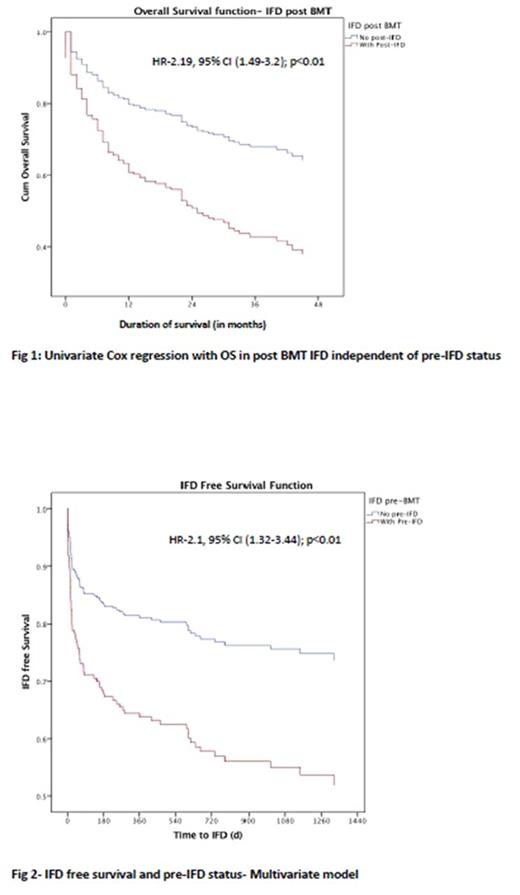
Results: Pre-IFD cases were similar to those without pre-IFD in gender, age, disease type, stem cell source, conditioning regimen and donor source whereas conditioning intensity, donor matching and HCTCI scores were significantly different. Significantly higher proportion of patients with EORTC defined pre-IFD developed IFD post HSCT (post-IFD); 35% vs 15% (p<0.01), with a significantly shorter median time to developing post-IFD (12days (IQR-0-42) vs 62.5d (IQR-14-403d; p=0.01). Similarly patients with pre-IFD had significantly higher ITU admissions versus those without (29% vs 18%; p=0.03), but this did not appear to be related to the development of post-IFD (p=0.62). ITU admissions were also significantly more in patients (n=70) who developed IFD post-HSCT (38% vs 12.7%; p <0.01), reflecting their significantly reduced cumulative overall survival (HR-2.19, 95% CI (1.49-3.2); p<0.01), but without any influence of pre-IFD status (HR-1.16, 95% CI (0.75-1.80); p=0.76) (Fig 1). There were no significant differences in overall survival between patients with or without pre-IFD (p=0.34) in keeping with reported similar survival estimates in EBMT study, although a trend for slightly higher survival beyond 5 years was noted without pre-IFD. Multivariate analysis confirmed pre-IFD status (HR-2.1, 95% CI (1.32-3.44); p<0.01) as single most significant factor negatively influencing IFD free survival post HSCT (Fig 2). T-cell depletion (in-vivo) using campath /ATG appeared to have a protective effect on IFD survival compared to haplo/cord blood or standard HSCTs (HR 0.21, 95% CI (0.51-0.88); p-<0.01). Finally pre-IFD status had no influence on NRM, OS and GVHD incidence estimates. High HCTCI scores, male gender, relapsed disease, absence of GVHD and post-IFD status were the most significant factors influencing OS.
Conclusion: Pre-IFD remains a significant challenge in terms of high post-IFD risk with an increased risk of morbidity with ITU admissions and related healthcare costs, although no difference in OS or NRM was seen overall. Although pre-IFD status is no longer an absolute contraindication for HSCTs, careful patient selection with aggressive treatment of pre-IFD patients and use of routine therapeutic drug monitoring to reduce prophylaxis failure is likely to help improve HSCT outcomes.
Raj: MSD: Speakers Bureau; Bloodwise: Research Funding; Mallinckrodt: Speakers Bureau; Celgene: Speakers Bureau. Potter: Pfizer: Other: Advisory board; Jazz: Honoraria. Pagliuca: Basilea: Honoraria; Pfizer: Honoraria; Astellas: Consultancy, Speakers Bureau; Jazz: Honoraria; Gilead: Honoraria; Merck: Honoraria, Research Funding; Bluebird: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal